Pediatric Intensive Care Unit Treatments

- Intubation and Ventillation
- Central line insertion
- PICC line insertion
- Intercostal drainage
- Nose and Ear foreign body removal
- Functional Echo
- Lung USG
Procedures
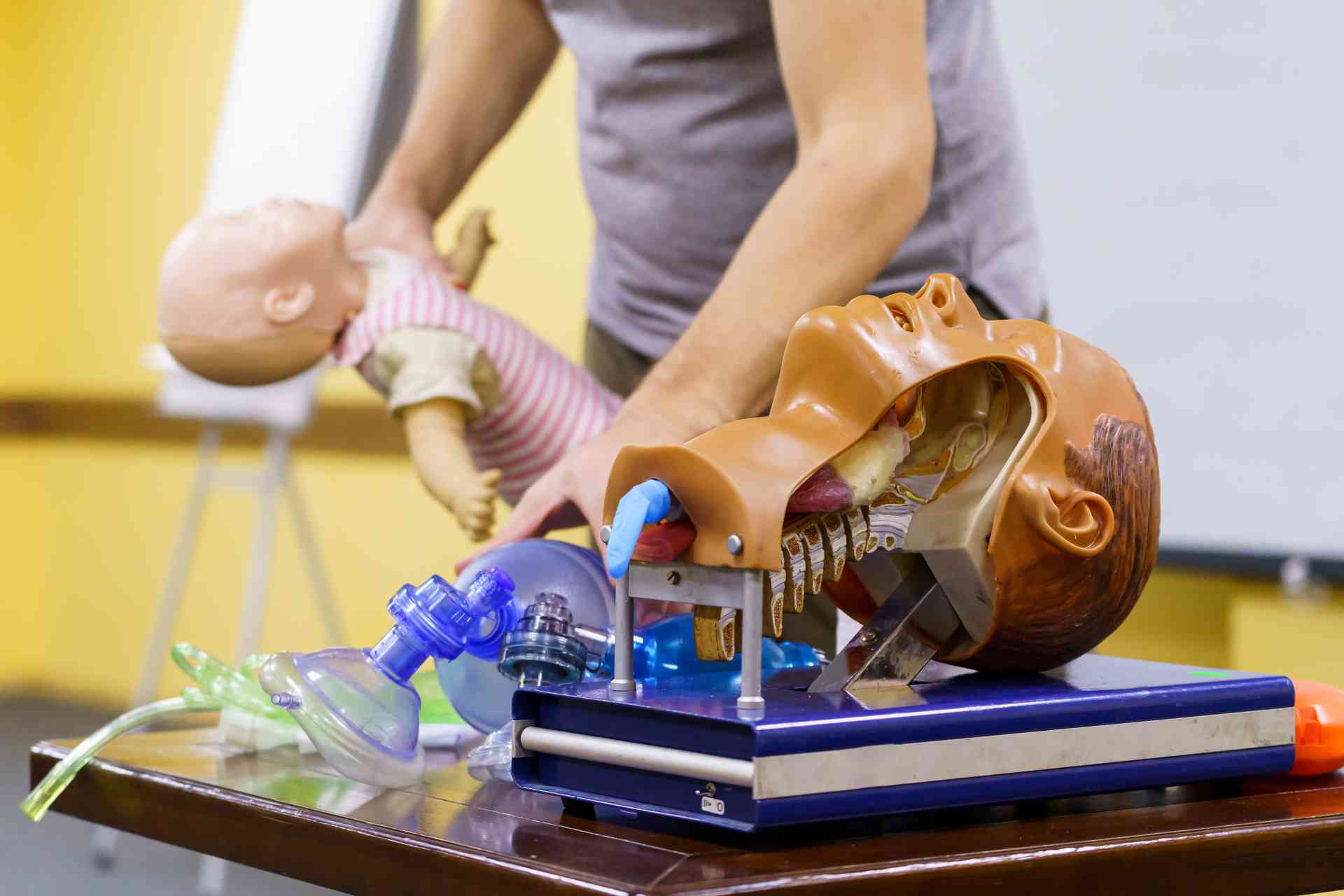
Intubation and Ventilation
Mechanical ventilation is one of the crucial aspects to save a kid’s life. To mechanically ventilate a baby or kid, a specialized respiratory machine is used to help pass the air in and out of the lungs to assist in breathing. To connect the kid’s lung to a ventilator, the Pediatrician intubates the kid.
Intubation is the process where a thin plastic tube is inserted into the windpipe through the mouth.
 When are Intubation and Ventilation needed in a child?
When are Intubation and Ventilation needed in a child?
Intubation & ventilation is needed in a child when the child is unable to breathe on its own.
Unable to breathe condition can arise due to multiple factors like:-
- When severe respiratory problems & emergency treatment are called upon, then the pediatrician needs to intubate and ventilate the kid.
- Many a time, the child won’t be able to breathe on its own while she/he is sedated during surgery.
Sometimes Severe asthma attack won’t let the child breathe on its own. Also during a serious viral disease, any serious injury or near-drowning experience requires intubating and ventilating the child, as in these conditions it becomes very difficult for the child to breathe naturally whether the child is conscious or unconscious, and immediate oxygen supply is needed.
However, pediatric intensivists have observed that in a few trauma cases, older children may receive air using a face mask or nasal tube if the airway is clear.
What to Expect after the procedure?
- Once a child is intubated, the pediatrician set the ventilator to pass air in and out of the lungs at desired volume and desired speed as per the need.
- Once the child’s condition improves and the child’s ability to breathe improves, the pediatrician will adjust the setting accordingly to wean the child off the ventilator gradually so that he/she can breathe normally without support.
How long a ventilator will be required to help in breathing for a child entirely depends upon the health condition and overall situation. The need for a ventilator may require a few hours to even months. The pediatrician weighs the situation and advises accordingly.
Central line insertion
A central line is a thin and soft tube (catheter) that is placed in a vein to deliver medications, fluids or other nutrients directly into a child’s bloodstream. A central line helps the child receive treatment with fewer needle pricks.
How does a central line help?
A child may benefit from the central line in the following ways:
- It stays in place for longer
- A child can get large amounts of fluids or medicines easily through a central line
- It can help the doctor take blood samples if required
Your doctor may take the decision of inserting a central line in your child in case he/she requires long-term antibiotics, has suffered excessive blood loss and needs large amount of fluids to be replaced, etc.
What to expect during the procedure?
- Before insertion of the central line, the child is given anesthesia, a medicine to make him/her sleepy so that they don’t feel anything during the procedure
- An ultrasound or an X-ray is used by the pediatric intensivist to identify the vein, after which a small catheter designed for children is put in place.
PICC insertion

Advantages of PICC line
- It can stay in place for a very long time (up to 3 months or more) and thus multiple insertions can be prevented in children requiring long-term therapy.
- Reduces the number of needle insertions in your child
- A large number of fluids and medicines can comfortably be given at once to children in such a case.
In which conditions can a PICC line help?
- In serious infections where intravenous antibiotics are needed for weeks
- Kids who have cancer, so that can receive chemotherapy and get blood tests done through it
- In children requiring multiple blood transfusions
- In children needing intravenous nutrition
What to expect during PICC line placement?
The following steps are followed during the procedure of PICC line placement:
- Area of insertion of the line is cleaned thoroughly
- Ultrasound is used as a guide for line insertion till a point near the heart
- A radiograph is taken to check the line after insertion
- A dressing is placed over the line after the procedure
When to call the doctor?
When at home with the PICC line, you can call your doctor if you notice:
- Fever
- Redness or swelling near the PICC line
- Pain or tenderness near the PICC line
- If the line gets blocked and cannot be flushed
Intercostal drainage (ICD)

What to expect during the procedure?
The following steps are followed during the procedure:
- An ultrasound or CT scan is done to evaluate the amount and location of the fluid.
- Your doctor will inject a numbing medicine at the site of the drainage.
- A small needle is guided through the skin into the fluid that needs to be drained.
- The fluid-filled up between the lungs and the chest wall is aspirated out with the help of a syringe.
- Your doctor may place a catheter at the site if continued drainage id required.
After the procedure, a small portion of the chest fluid taken out is sent for laboratory examination, to know the cause of fluid accumulation in your child.
Activity restrictions after the procedure
In case a catheter has been placed in your child for drainage of fluid your child will need to avoid any activities that can cause a pulling effect at the catheter. Children in whom catheter has not been placed can resume normal activities in a day or two after the procedure.
Nose and Ear foreign body removal

Dr. Vamsi Krishna has helped many young children by removing objects from the nose and ear.
What can get stuck in the nose and ear?
Anything small enough to enter the canal of the nose and ear can get stuck in it. Some common objects include:
- Insects
- Toys
- Buttons
- Small pieces of crayons
- Small batteries (button batteries often found in toys)
- Pieces of tissue
- Clay (which children play with)
- Small piece of Eraser
- Food
How can you know if something is stuck in your child’s nose and ear?
At times, objects placed in the ear may not cause any symptoms. However, some objects, such as food and insects, may cause pain in the ear, redness, or drainage. The hearing may be affected if the object stuck in the ear is blocking the ear canal.
The most common symptom in a child with a foreign body in the nose is nasal drainage. Such drainage appears only on the side of the nose where the object is stuck and often has a bad odor. At times your child may also have blood discharge from the nose
After careful examination, your doctor will remove the object stuck in the nose and ear using specific instruments to reach the inside of the nose and ear, and suction machines. Your doctor may also prescribe your child, ear drops, nose drops, or antibiotic ointments as needed.
Lung USG

How is the procedure done?
A transducer is placed over the skin of the chest which sends ultrasound waves inside at a frequency too high to be heard. These waves bounce back and the signals they produce generate the images of the organs within through computer-operated programs.
Your doctor will use an ultrasound gel during the procedure which is placed on the transducer and the skin to allow smooth movement and to eliminate any air between the skin and the transducer for best sound conduction.
Once the images are produced your doctor interprets the scan and gives you the report.
When can your child need a lung USG?
Lung USG can be prescribed by your doctor in case they suspect a problem such as:
- Lung pathology
- Pathology around the lung
- Shortness of breath in the child
- Severe cough
- Shock
Lung USG is a low-cost and effective procedure that can be performed on your child without any harm.
 When are Intubation and Ventilation needed in a child?
When are Intubation and Ventilation needed in a child?